by Diane Rufino, December 2022
My name is Diane Rufino and was 60 years old when my “story” began. This is me, below, just before it all started.

This is my cancer story.
It all started on October 17, 2020 when my family and I attended the wedding of our good friends Shane and Marnie. The reception was held in a banquet room in downtown Greenville. It was a fun affair, mingling with friends, making new ones, enjoying the food, and laughing at the antics of the newly-married couple.
Ah, the start of a new life together. It’s always one of the happiest days of one’s life and a joy for others to share in their bliss. My husband and children noticed a few things that were unusual for me – I didn’t want to drink any alcohol, even when celebrating the blessed union, and I didn’t take a single picture of anyone with my cell phone. But the one thing I did notice about myself was my sudden inability to walk down stairs and to walk stably in a straight line.
There were a series of steep stairs when leaving the venue and I was unable to walk down them without the help of my husband and one of my daughters. I thought it was strange since I hadn’t had a single libation. I simply chocked it up to the heels I was wearing. Yes, that had to be it. Then we got down to the street level and began walking to our car. That’s when I really noticed that something might be wrong. I kept stumbling and weaving back and forth. My husband Doug became nervous and physically had to hold me tight as we walked for about a block in distance. I was repeatedly asked: “Mom, are you OK?” Doug asked the same question.
Two days later, Doug called our family doctor and told him of my unusual behavior, and the doctor advised that he take me to the Emergency Room at Vidant Medical Center for an examination and for a series of tests. And so, on October 19, Doug brought me to the Emergency Room. There, I was given a bunch of tests, including blood, urine, and various scans.
As I sat in one of the curtained stations, I was relieved that everything was looking fine. But then, a young male doctor opened the curtain and pronounced: “We know exactly what the problem is. You have a large brain tumor behind your left eye.” He then showed us the scan. I remember saying: “Oh no, that’s not good” and then the doctor scurried Doug away to have a consult with him. It was at this time that a nurse gave me something in an IV and after that, I can remember nothing.

I woke up in the hospital, being kept in a groggy state of mind with drugs. There were nurses coming in and out of my room, taking stats and giving me more drugs. Doug and all of my children took turns sitting with me, from sun up until night time. The doctor came in my room to explain what was wrong with me. He said I have a grapefruit-sized tumor called a meningioma, which is a tumor of the meninges, the membrane lining around the brain. It was so large that it was pushing into my brain. It needed to be surgically removed immediately. “Don’t worry, Mrs. Rufino,” he said, comfortingly, “these types of tumors are overwhelmingly benign. Once we remove it, you shouldn’t have to worry about it anymore.” I felt comforted and dozed off, as usual.
I imagine he told me when the surgery would be scheduled but I have no recollection of that. All I remember is that in the middle of the night, I felt myself on a stretcher and being wheeled around the hospital. But I nodded off again. Then I remember a technician telling me that I was fidgeting with my hands and I would have “to have another scan taken.” I remember that second brain scan.
As I mentioned, I have very little memories of those early days in the hospital. My daughters apparently braided my hair and took a picture of me smiling, which they showed to me. I don’t remember them taking it. I would come to cherish that picture because it was the last one with my long straight hair, the last picture before that hair would fall out.


The surgery was scheduled for Thursday morning, October 22. It was supposed to take 8 hours but only took approximately 5 hours. I woke up in recovery and my family was there to greet me. I had a bandage across the top of my head. There were 68 staples in my skull, but I felt no pain or discomfort.
Within the hour, I was moved to a small room in ICU. There were no windows; just a bed and a sink with cabinets. I remember my hair (beyond the bandages) felt hard and matted and my face a bit swollen. I didn’t dare attempt to look in the mirror. I remember the nurses asking Doug if he wouldn’t mind bathing me, which meant to wipe me down with large body wipes. And I remember the nurses picking me up and putting me on a metal toilet seat to go to the bathroom. But the one memory that really stands out is the one that helped me break up the monotony of sitting in my bed with nothing to do. I would ask the attending nurse if she would walk me just outside the room to the window where there was a chair and I could look out onto the bustling life of Greenville. All I did was sit and look, but for me, it was everything. It was enough to get me through the monotonous days.


My husband spent most of every day sitting at my bedside. He would talk to me and occasionally put on the TV, and sometimes I would see him crying. He would leave around dinner time to go to the cafeteria to get something to eat. Most days, he would bring me something back from the cafeteria, like chicken tenders and fries, or grilled cheese sandwiches and soup. He liked to bring me food, and often, he would eat it himself. That was Doug. He was so protective of me and as God is my witness, I was left alone in my room no more than 1-2 hours each day. He literally spent each night with me, sleeping in the reclining chair in the room. Every once in awhile, one of my children would come to visit and sit with me. I was unable to speak so I thank God with my whole heart for the family I have been blessed with. They were so determined and loyal and committed to me and my healing process. Most of all, they were so strong and supportive.
My sister paid a surprise visit while I was recuperating in the ICU. I was in and out of consciousness and I remember very little of her visit. I couldn’t speak and felt so bad about that. I remember looking at her and seeing her break down and cry. It was heart wrenching. And then my best friend Karen came to visit. She has a heart of gold, a huge heart. She came to support me and to let me know that she cares. She herself suffered a brain tumor a few years earlier, but went to John Hopkins for a few months for treatment. As with my sister, I remember Karen bringing a chair right up next to my bed and talking to me. She asked me lots of questions, and again, I was unable to articulate words. I nodded or shook my head. It was the best I could do.
Within a week, I was moved to the Rehabilitation wing of the hospital. I was able to speak by then, but very minimally. And I don’t believe I was able to articulate sensibly. And I was very unstable on my feet. I would need to be rehabilitated on my speech, my cognition, my ability to move and walk, and my ability to go to the bathroom on my own and to take showers. Apparently, I was not an easy patient during my weeks in Rehab. I was told that I gave the nurses a hard time when it came to taking medication and having the incessant tests taken. I have no recollection of that at all. I’m usually a very calm and compliant patient. In fact, on my chart, there was a notice of my reticence, my rebelliousness. The nurses and doctor had to contact my husband about the issue and he told them to either put the medication in my IV, if possible, or disguise them as a sugar pill or melatonin for sleep. I remember hating the steroids they were giving me. I felt they were giving me hallucinations.
As with the ICU, Doug would spend all day with me, religiously and unceasingly, and then one of my four children would come back at night to keep me company. They would take turns, and from what Doug told me, they eagerly took turns.
I especially remember a night when Sierra, my second daughter, came to visit and was talking to me and I was unable to answer her. I just couldn’t articulate anything. I began to cry and she hugged me and said it wasn’t necessary for me to answer and talk to her. In that moment, I felt such love from her, as with all my children, and from Doug as well. Sierra would bring me Italian food and Italian desserts, and just as Doug often did, she would eat them.
And another night, my son Hunter came to visit, bringing me Chinese food – my favorites. Apparently, I gave the nurses a hard time about taking my medication (I don’t remember doing that) and so, he called his father. Doug called the hospital and told them to do whatever they needed to do but to make sure I took all my meds. I soon realized what Hunter had done and got angry, accusing him of “throwing me under the bus.” I remember telling him to leave. “Go home!” I told him. And angrily, he left. About 2 minutes later, he came back in my room, packed up the Chinese food, and said to me: “And I’m taking the food too!” Ouch.
Then came the day when the nurses had to show me how to shower safely. One of the nice nurses helped me undress and then walked me into the shower, making sure that I sat properly on the shower chair. The first thing I noticed was all the bloodied water coming off my head. My mind went to the Alfred Hitchcock movie Psycho and its famous shower scene. I looked at my pathetic body and saw how withered my legs had become and how skeleton-like I now appeared. I remember trying to count the number of days I had been in the hospital, immobilized, causing such a frail and withered appearance. And then I wondered if, and when, I would regain my musculature and my former body.
After I was done with the shower, another nurse joined us to try to comb out the matted mess that had become my hair – my remaining hair, that is. Yes, it took three of us to come through and remove all the matted areas of my hair. It took quite a long time and there was a lot of long hair in the wastebasket. I couldn’t have realized at the time how much I would come to miss all that hair.
I spent my time in the Rehabilitation wing getting stronger, hopefully putting weight back on (my body had decayed into that of a 90-year-old woman), learning how to go to the bathroom on my own and taking a shower (albeit with a nurse), learning to walk again, lifting some weights, and eventually working with speech and cognition technicians. I remember one afternoon when Doug was visiting with me, I had a session with the cognition technician. Doug went with me. The technician asked me some simple questions, and although I knew how to answer, I was unable to articulate them. I looked at Doug and started to cry. I guess it would take time for my brain to recover.
The following day, Dakota, my third daughter, came to visit and she accompanied me to my session with the cognition technician. Again, the technician asked me some fairly simple questions and again I was unable to articulate appropriate answers. This time it was Dakota who started crying.
As the days went by, however, I realized I was getting better. In fact, each day was becoming exponentially better for my brain. That’s when I realized that I still had a brain and that it would still be functional. It was now the week of November 9. It was starting to look like I might be released from the hospital soon.
And then it finally happened. A nurse came in to my room on the morning of Thursday, November 6, 2020 and removed my staples (not fun) and very soon after, the doctors examined me and I was released from the hospital. I’m sure they were glad to get rid of me. But rehab wasn’t yet complete. I was scheduled for rehab sessions, physical and cognition, from Monday through Thursday, November 16-19. I did well enough that I would not be required to return for any further rehabilitation.
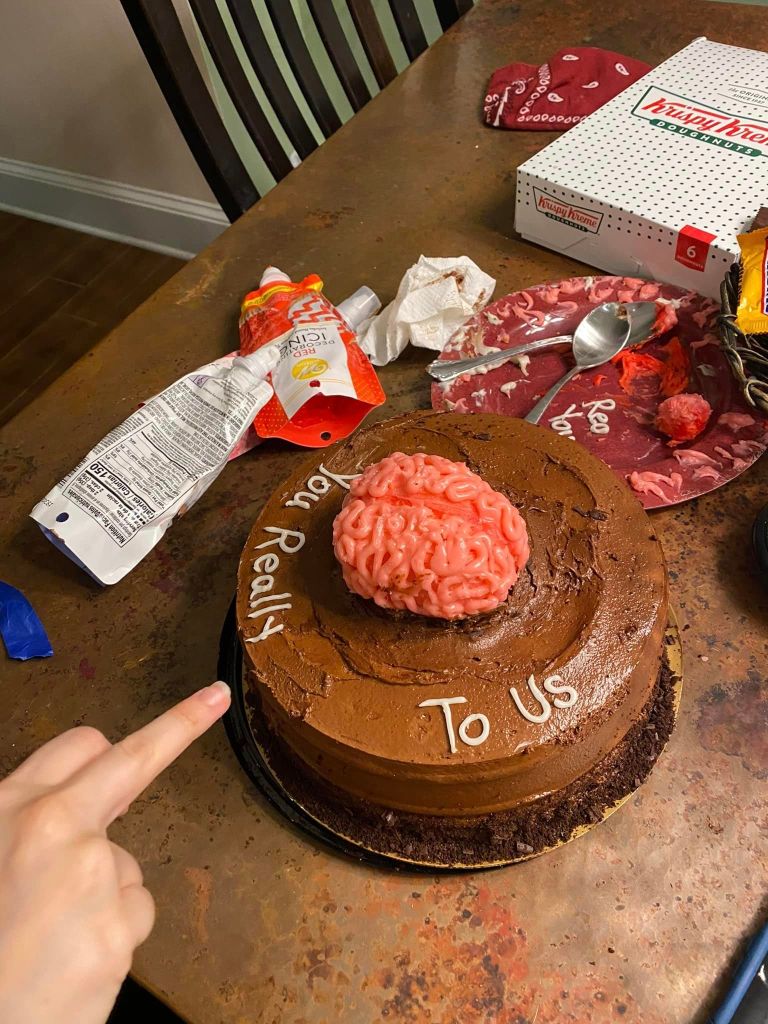
I arrived home to a house filled with balloons and a home-made banner reading “WELCOME HOME.” Doug rearranged our bedroom so that the bed was flush against the wall. He didn’t want to take the chance of me falling off in the middle of the night. And my daughter Sierra made me a very special cake, which will always stand out in my memory.

On Friday, November 13, I had my first post-op consultation with my lead oncologist, Dr. Stuart Lee, head of the Gamma Knife Center at Vidant. I remember this meeting vividly. Dr. Lee, who is certainly one of the nicest, most down-to-earth physicians I’ve ever met, walked into the examination room and sat opposite from me. I can still recall how he was unable to look me in the eye. I instantly knew there was bad news. And then it came: “I got your path results. It couldn’t be worse. You had a class 3 malignancy. It’s an especially aggressive form of meningeal cancer.”
The first bit of news that changed my world was the announcement “You have a large brain tumor behind your left eye.” And now, the revelation that it was an aggressive form of cancer. Any optimism I had for a complete recovery was shot down. Any optimism that I would be a cancer survivor was immediately shattered. To make matters worse, Dr. Lee reviewed the scientific literature on malignant meningiomas for us. For the kind of tumor that I had, which is extremely rare and extremely aggressive, there would be a very high probability that it will re-appear within a 3-year period. I would need to go for routine (every 3 months) MRI scans, with a contrast agent. He explained that scrutinous monitoring of my head would be the best way to stay on top of my treatment.
Dr. Lee told Doug and I that he would hold an all-day consult session the following Monday, November 19, with his (my) oncology team – Dr. Jasmine Jo, Dr. Hyder Arastu, and of course, Dr. Lee himself, to come up with a treatment plan. He led us to believe that radiation therapy would be needed. He said he would let us know.
On the afternoon of November 19, we got a call from Dr. Lee letting us know that radiation therapy was advised by Dr. Arastu, the radiation oncologist (a physician with over 35 years of experience in treating brain tumors). As he explained to us, there is no known chemotherapy that has been shown to be effective for treating a malignant meningioma, but radiation would most likely will do the trick. Radiation, he said, is used to kill any cancer cells that may be left behind after surgery. He re-emphasized that he believed he excised the entire tumor during surgery. He went on to explain that radiation can potentially affect wound healing, and so treatment might need to wait for another 2 weeks. Dr. Arastu would make that decision. Finally, he told me I would need to go for an MRI the following Monday, November 23, to set measurements for that therapy. I was scared on one hand but hopeful that Dr. Arastu, with his expert experience, would take good care of me.
Thursday, November 26, was Thanksgiving and I felt so very blessed to have caught my cancer in time, to be alive, and to be with my family. This was the most special of all Thanksgivings. My children were amazing. They made all the holiday foods that I love and at the table, they each said a prayer for me. After weeks of dismal hospital food, the Thanksgiving feast was a delightful treat to my palate.
The following day, November 27, I officially began an exercise regimen to work my deteriorated muscles and to hopefully get my legs and arms back into shape. I was in bad shape, to say the least. I couldn’t walk with stability, I couldn’t walk up and down stairs, I could bend down but not be able to get back up, I would often fall off the toilet, I needed to have one of my daughters walk me into the shower and sit me on a shower chair, and I couldn’t hold a pen in my hand or write. Aside from these limitations and debilitations, I didn’t have any horrible side-effects from the surgery except for a bad mid-afternoon headache and severe anxiety attacks around the same time.
My exercise regimen included a series of leg lifts and leg stretches, a walk around the neighborhood (1.5 miles), and 5-lb weight-lifting. Everything was so tough. Whenever I got an anxiety attack, I would ask one of my children to walk with me around the neighborhood. The walks seemed to help quite well.
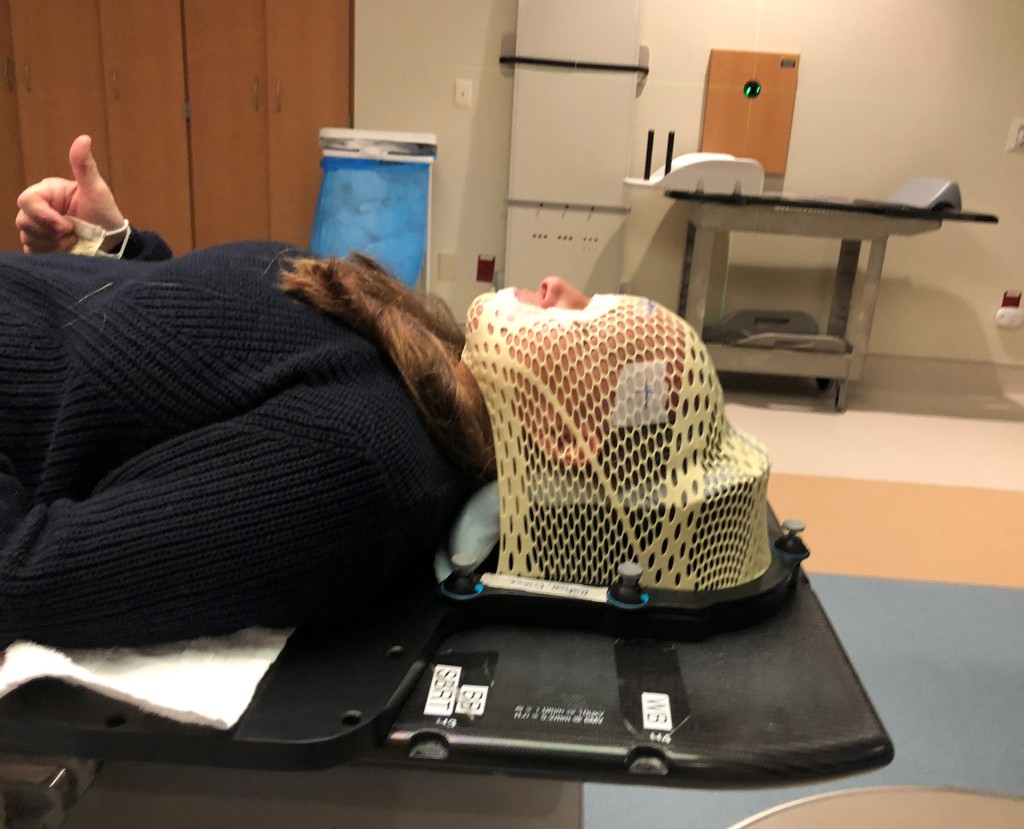
On Monday, November 30, I was scheduled to go to the Vidant Cancer Center to have a mask made for my radiation treatment. The treatment would involve having a tight mask (formed precisely to fit the contours of my face) placed on my face, bolted to a table which would hold my head in place and would then be moved mechanically into the radiation (X-ray) machine. The mask procedure was simple. They placed a heated mesh mask over my face, formed it to my face, and let it set for a few minutes to harden.
Next, I was sent to another wing of the hospital to have a CAT scan.
When I came home from the hospital and for about two weeks after that, I remember having bad days. By “bad,” I mean that I had low energy, had trouble sleeping (only able to get between 3-4 hours of sleep each night, with hallucinations from the steroids), and trouble walking and getting around. In those two weeks, I only had 3 “good” days, meaning that I finally had some energy.
The following week is when I started to make an effort to start walking around the neighborhood. I felt weak walking down the five stairs and often my legs would collapse while doing so, I had little energy and ability to climb up those stairs, and I even felt weak walking up and down curbs. Why did it take so long for my muscles to rebound back to the shape they used to be?
Once I began my exercise regiment, however (even though it was minimal and gradual), I noticed that I had more control walking around and climbing up and down the stairs. I actually felt myself finally getting stronger. Also, I began to notice that there were fewer bad days and more good days.
On Wednesday, December 9, I went for an MRI at the Cancer Center for the purpose of finalizing measurements for the radiation treatments, followed by a consultation with Dr. Lee. He finally gave me some good news. He said my recent CAT and MRI scans looked good and showed remarkable progress; that is, remarkable healing of my brain. With the tumor gone, my brain, which had been compressed, began to move back into place. I asked him: “Will the space fill up with new brain cells? “Sorry, Mrs. Rufino, it doesn’t work that way,” Dr. Lee replied.
Dr. Lee showed Doug and I comparison scans, ones taken right after my surgery and the ones taken on November 30. He also told me that my radiation treatment would have to be delayed for about one week because Dr. Arastu was waiting for a nuclear physicist to review his plan. He wanted to be sure that I could handle the amount of radiation he was planning and also, because the tumor backed up behind my left optic nerve, he wanted confirmation that the radiation dosage would be appropriate.
Friday, December 11, I was scheduled for yet another CAT scan – a final CAT scan – to finalize Dr. Arastu’s radiation plan. It was to be done with the mask on. Unfortunately, I had a full-blown anxiety attack when the mask was put on. The mask was very tight, it covered my nose, and when they bolted it to the table, I felt as if I could not breath easily. I immediately panicked. My heart rate became elevated and I signaled to the technician that there was a problem. I started crying like a baby and told them I couldn’t go through with it.
I felt like I let my family down and I felt like I let my oncology team down. All along, everyone kept telling me that I was a fighter. Now I felt like a loser.
But on my way out of the hospital, I got an idea. I stopped off at Dr. Arastu’s department and asked to see him. He was not in, but an associate would be able to see me. I asked if he could look at my mask and alter the area around my nose. Since the mask was intended to keep my head perfectly still, I figured (I hoped) that they could cut a hole out for my nose. The young doctor said that was a good solution. He also suggested that I ask the doctor for Lorazepam, an anti-anxiety drug.
With that, I was scheduled to start radiation therapy on Monday. If the mask was suitable and if the Lorazepam worked, I would first have the CAT scan and if all looked good, I would have my first radiation treatment. In the meantime, I had gone to see my family doctor and brought him up to date on my cancer diagnosis, surgery, and now my impending radiation therapy. He thought my blood pressure was running high, and so he prescribed me the drug Metoprolol which is supposed to address both my blood pressure and anxiety issues.
When I got home that afternoon, I got a call from Dr. Arastu’s office. He had prescribed me Lorazepam, which was ready for me at my local Pharmacy and I was instructed to take one (1 mg) tablet 30 minutes before every radiation treatment.
Monday, December 14 arrived. Doug went with me to the Cancer Center and as it turned out, the CAT scan went just fine. The mask had been altered as I had requested and I had no problem with anxiety. I’m sure the Lorazepam took the edge off, as it was designed to do. The first radiation treatment followed and surprisingly was simple and easy. In fact, I would come to look forward to each treatment because I would be able to rest and relax. Sometimes I would even fall asleep. I had daily radiation treatments, and each one was without incident. I had a day or two off, due to the Christmas holiday. By the end of December, I was more than one-third of the way through my radiation treatment.
From about 3 weeks or so after returning home after the surgery, and even before radiation began, I was back to thinking clearly, rationalizing intelligently, and writing my articles. In fact, if I would be so bold as to toot my own horn, I would say that some of my best and most thoughtful and intelligent articles were written in the months of December through March, 2021.

My treatments resumed on Monday, January 4. The following day, after I returned home, I marked my calendar “HALFWAY DONE.” I was excited to have reached that point. On Wednesday, I had my weekly consult with Dr. Arastu and he was very pleased with my progress. He told me that I am a “model patient.”
It was around mid-January, that I began getting bad headaches at around 7:30-8:00 pm followed by bad anxiety attacks. This would mark the first time since my surgery that my head hurt. I called my family doctor’s office with the news and the doctor quickly called me back advising me to take a single Lorazepam tablet (1 mg) before going to sleep.
The headaches and anxiety attacks continued after that, each one at almost the exact same time. Even though it was very cold outside, I would pack on my coat, a scarf, mittens, and my boots, and walk around the neighborhood. One tour was usually good enough, but several times, I needed to walk it twice.
The side-effects from the radiation were getting worse. Now I was having problems sleeping and my appetite was waning. My body would be exhausted and I wanted badly to get a good night’s sleep, my when I put my head on my pillow, my mind would race and I could not fall asleep. On Monday night, January 18, I needed to take 2 Lorazepam tablets to sleep. And even at that, about 3-4 hours later, I was wide awake again.
On Wednesday, I had my weekly consult with Dr. Arastu. I told him about my recent problems sleeping and my loss of appetite. He told me to make sure I eat at least 2 times each day, with healthy food items and to keep doing what I was doing for sleep. He said that the only problem, if at all, from the X-ray treatment might be a mild impact on my immune system. I may be mildly immune-compromised, he said, but that wouldn’t explain my symptoms. He comforted me by telling me that within a week of the last treatment my immune system would be back to good.

Wednesday, January 27, was the most meaningful of calendar dates – It was my last day of radiation treatment!! The technicians were all so kind and wonderful and they made the session very special for me. After the session had ended, they handed me my mask (and told me I could keep it, like I really wanted that) and walked me to the radiation bell. I got to ring the bell, the tradition in radiation oncology when a person completes his or her course of radiation treatment, and pictures were taken, both for me and for the department. Dr. Arastu sent me on my way, with optimistic remarks and messages of hope. He reinforced that I had been an exceptional patient and explained that the radiation treatment would stunt the hair growth on the front of my head (the exact target of the radiation) but that within 2 months I should start seeing the hair grow back in. He warned though that its texture may not be the same.

Immediately, I went out and got a hair “re-growth” formula to apply to the front of my head. I got Nioxin “Hair Re-growth Treatment.” The instructions were to apply to the front and sides of my head twice each day – in the morning and then again before I went to bed.
On Saturday, Doug took me out for a fun day – to spend it however best would make me happy. I love animals and so I suggested that we go to New Bern, walk the waterfront and feed the ducks and then walk downtown and visit the local shops and perhaps even stop for ice cream. And so that’s what we did. It was a perfect day. We enjoyed the ducks, enjoyed strolling through the antique shops, and enjoyed some ice cream. My favorite exhibit of the day was the large Elvis statue. Visitors to the antique shop were singing his songs and doing their best imitations. My sickness, at least for the day, was behind me. With my hat on, to cover the scar across the front top of my head, I felt normal and was grateful to spend such a perfect day with my husband. I felt blessed.

Healing from the radiation treatments was the toughest part of my cancer ordeal. No one had prepared me for what was to come. Some of the side-effects included bad headaches, very sensitive eyes (I had to wear dark sunglasses), swelling on my face (particularly around my eyes), increased anxiety attacks (where I would need to walk outside around the neighborhood), a complete loss of appetite, and an inability to fall asleep at night. It was so absolutely frustrating to try coming up with schemes to pass the night away while being unable to sleep. I would take 1-2 Lorazepam pills but that would help only temporarily, if at all. I would wander around the house and our property endlessly, looking for a new place to try to sleep – the living room couch, my office couch, the lazy boy reclining chair, the bed out in our pool house, and even the couch in the pool house. It was exasperating and never helped. Next, I got an Alexa device and loaded it with soft music such as movie themes and other classical pieces and would play that to calm my mind, then I often would play hours of solitaire in bed, and then there were nights when I simply put on the TV and watch movies or walk on the treadmill that Doug had bought for me or soak in the tub with eucalyptus stress relief soap. Nothing really helped. By morning time, I was physically exhausted. I would wait until the afternoon when the bad headaches and anxiety hit, when I would take my Lorazepam, to try to nap and catch up on sleep.
I would need to bring this issue up to my family doctor and see if there is a sleep-inducing agent that I might try, although my nature tells me to avoid medication in general whenever possible. And so, I went to talk to my doctor. He advised that I try Melatonin instead of Lorazepam, but I told him that I was given plenty of Melatonin in the hospital and it never worked. He then suggested I try Ambien, which he prescribed, which is the same sleep drug that my father used to take which worked like a charm for him. I tried it for a few nights, but each night, instead of helping me fall asleep, it made me more energized and even more unable to sleep. In fact, I got the jimmy-leg and was really miserable. Next, he prescribed Lunesta (Eszopiclone, 2 mg tablets) which also didn’t work. It did the same thing – gave me added energy rather than help me ease into sleep. It also gave me the ”jimmy leg.” Next, he prescribed Belsomra (Suvorexant, 15 mg tablets). I followed the doctor’s advice and took the drug religiously for 7 nights. Again, it was ineffective. Unlike the other sleep drugs, it caused bad headaches, and unlike the other drugs, it didn’t give me the “jimmy leg.” Thank God for that, at least.
Finally, he prescribed me a new sleep aid (a fairly new drug), Dayvigo (Lemborexant). As instructed, I took the drug for 7 straight nights. As usual, it was, for the most part, ineffective. Like Belsomra, the side-effects were terrible. It gave me bad headaches.
That ordeal took me through the second week of March, 2021. I decided I would give up on using any sleep aids.
By the second and third weeks of February, I began to notice that my hair was starting to fall out by the handful in the shower. This could not be! No one told me this would happen! As the days went by and the hair fell away, I knew the inevitable would soon become a reality. I would lose all my hair. And so, on March 3, I took matters into my own hands. I took my husband’s beard shaver and shaved the remaining hair off my head. What a sad day. I loved my long hair. Bye bye long thick hair.
On Tuesday, February 23, I went for my first official post-radiation follow-up MRI, followed by a consultation with my new lead oncologist, Dr. Jasmine Jo, a petite sweet Filipino doctor. Dr. Jo told Doug and I that my MRI scan looks spectacular. She said that it appears that I am healing very well and that there is no evidence of any tumor re-growth. She also gave us some more good news…. I would not need to be on the steroid drug Keppra any longer. Keppra was given to me in the hospital (and then later prescribed) to prevent brain swelling. She advised, from her research, that Keppra was not especially effective and that the side-effects, the hallucinations, outweighed its benefit.
On Wednesday, March 17, I finally began to drive again. It felt so wonderful. I began to start feeling some degree of independence again. Up until this point, I was under the scrutinous eye of Doug and all my kids. I was hardly ever by myself. Someone was always around to watch me, walk with me, take me into the shower, and help me clean. My family didn’t even want me in the kitchen to cook.
I suffered through endless nights of “jimmy leg” and an inability to fall asleep. I thought the torment would never end. I was going through hell, for sure. Again, no one told me to expect this and no one even told me about it.
On Thursday, May 20, I went for my second post-radiation MRI. That afternoon, I had a very bad headache – the worst one I have had in a long while. I took a Lorazepam tablet and thankfully, it went away. That night, I was unable to sleep even a wink because of a bad anxiety attack. I couldn’t remember the last time I had such an anxiety attack at night. I took another Lorazepam tablet but it didn’t help at all.
I called my family doctor on the 24th and told him about my sleep issues, and he suggested I try Trazodone, the drug that he himself uses to sleep. It is non-narcotic and apparently non-addictive. He prescribed me a 30-day supply of 50 mg tablets. I tried one that evening and it worked like a charm. A sleep aid that finally works! It was a miracle.
I was bald and finally able to sleep, thanks to Trazodone. I was finally happy. The weather was starting to warm up and so Doug took me to one of my favorite places – the beach. It was a glorious day. We even went out to eat at Havana’s at Carolina Beach before returning home.

I had consultations with both Dr. Lee and Dr. Jo the following week and both said the MRI scans of last week looked very good. Dr. Jo went into more detail. She showed me on the scans where there was some slight scarring along the periphery of the surgical excision, indicating some thickening of the myelin sheath, but explained that scarring was to be expected from the type of intense radiation treatment that I went through.
On July 9, I made a personal decision to wean myself off of Lorazepam. For one week, I would take 3/4 of a tablet, the following week, I would take only 1/2 of a tablet, the following week I would take only 1/4 of a tablet, and then the fourth week I would not take any at all.
For the most part, I plan worked out well. Occasionally, I suffered a bad headache, and with the Trazodone at night, I was getting a good night’s sleep. On Sunday, July 18, I traveled with my family to Raleigh to the NC Museum of Natural Science and the adjoining new science museum. We love museums and we especially love the science ones. After our afternoon at the museums, we went to an authentic Italian restaurant in downtown Raleigh for dinner. It was excellent. Such a treat. It was such a perfect day.
By the start of August, I had weaned myself off of Lorazepam. It was such a great personal achievement, and I was proud of myself.
Meanwhile, my hair started growing back in. Unfortunately and unexpectedly, it came back in white and course as hay. A further insult to my poor body! On August 21, my eldest daughter Cheyenne dyed my hair. She went to the beauty store and picked out a professional-grade medium brown color. After she finished doing my hair, however, it turned out to be closer to black. I was not happy. I eventually went to a beauty parlor, had it re-colored and had blond highlights put in it. What a difference a color makes!
On Tuesday, August 24, 2021 I went for my third MRI scan and then a consult with Dr. Jo. Again, the scan was good, didn’t show any re-emerging tumors, and showed that my brain was continuing to heal well. As Dr. Jo told me: “You continue to be cancer-free.”
December 9 would be my last MRI of the year 2021. As before, the scan showed no remnant of the pesky cancer and showed continued healing of my brain. Dr. Jo was so convinced of my recovery that she moved the frequency of my MRI scans from every 3 months to every 6 months. I was settling into a comfort zone, believing it just might be possible that I would be among those lucky individuals who could claim themselves to be “cancer survivors.”
But I was a little too optimistic, as it turns out. On Tuesday, May 31, 2022, I went for my scheduled MRI and the results were terribly disappointing. Sitting in the consult room with Dr. Jo, she showed Doug and I the scan and pointed out where there were 2 new small tumor. Each were calculated to be less than 1/2 inch in diameter, she said. My world collapsed. Reality set in. To be honest with myself, the results were not unexpected and I should have expected it. The tumors were at the top of my head, above my left eye.
I immediately began to cry. I was no longer a cancer survivor but was once again, a cancer patient. I told myself and Doug that I could not go through brain surgery again. I felt that I had enjoyed a wonderful life and if my time was up, then it was God’s plan. Doug was devastated. Dr. Jo did her very best to comfort me. She said that surgery would not be needed and that a fairly new procedure known as Gamma Knife Surgery would likely be the preferred course of treatment. As it turns out, Dr. Stuart Lee is the head of the Gamma Knife Center.
The following day, June 1, my oncology team met to discuss my case and concluded that indeed, Gamma Knife would be the best procedure for my recurring little tumors. As explained to me, Gamma Knife is a non-invasive stereotactic radiosurgery instrument that involves no scalpel or incision. It uses precisely focused beams of gamma radiation to treat small malignant and benign brain tumors, without harming surrounding healthy tissue. Gamma Knife treatment is often preferred because it offers several benefits over traditional surgery because it is painless and often an outpatient procedure, and it treats with pinpoint accuracy.
OK, I felt a lot better.
On Tuesday, June 7, I arrived at the Gamma Knife Center at Vidant Hospital for my Gamma Knife procedure. Doug and I went into the prep room where I was seated on an examination table and set up with an IV. I was given an oral dose of valium (10 mg) and almost immediately, Dr. Lee began to apply a numbing agent to the top quarters of my head. He was preparing me for the head brace that would have to be screwed into my head to hold the “radiation helmet” which has hundreds of pin holes in it to focus the gamma radiation on my tumors. I don’t remember him actually screwing that head brace in. I only remember the nurse giving me an injection of Versed and then another nurse helping to lift me off the table and into a wheelchair. Then I went blotto. I was out like a light. I was eventually wheeled into the adjoining “radiation room” for the actual procedure, which took 65 minutes.
The next thing I remember was waking up as I was being wheeled into the recovery room. The brace was still on my head. As soon as I got into the room, the technicians unscrewed the head brace. When I touched my forehead, I felt 2 swollen knobs. They were hard as a rock. A nurse put an antibiotic cream on the sores (2 on my forehead and 2 on the back of my head) and called in a prescription and sent us on our way. The procedure I had been so nervous about was over. It turned out to be a piece of cake….. because, of course, I was completely knocked out for it.

About a half hour later, the numbing agent wore off and my head – those areas where the head brace was screwed in – began to hurt badly. I went home and slept for a few hours and then all was well.
On August 2, I had a post-Gamma Knife MRI scan and then a consult with Dr. Jo. The scan, she said, looked just fine, as they expected. On Tuesday, October 25, I had my second post-Gamma Knife MRI scan. Again, the scan looked very good. There were no new growths and the small tumors that were irradiated and killed by the Gamma Knife had disappeared.
That completes my story as of 2022. I will go into the new year with an MRI schedule that will scan my head every 3-months, and I feel good about that. The earlier any new growth is detected, the better and quicker it can be treated. Maybe there is still a chance that I will become a “cancer survivor.”

I dedicate this story to Doug and my children – Cheyenne, Sierra, Dakota, and Hunter. I love them all with all my heart.
